Abstract
Background: In June 2016 the Yale Sickle Cell Disease (SCD) Clinic began to certify adult patients for medical marijuana (MM). Illicit marijuana (IM) use is common in patients with SCD and most who use it feel it treats their pain. While there is limited data on the efficacy of marijuana for SCD-related symptoms, our team opted to certify patients due to speculation that it would be safer based on improved regulation and reduced legal risk of MM compared to IM.
We designed a survey to assess why and how participants used IM and MM and how they felt the two substances compared with respect to SCD-related symptom management. We hypothesized that most participants who were certified for MM had been previous IM users who felt that marijuana had a positive effect on pain.
Methods: All patients were educated on safety risks of MM before certification. After certification patients were required to submit regulatory documents the state of Connecticut and pay a $100 annual fee prior to obtaining MM from dispensaries. Patients who had been certified for MM at our clinic were contacted by phone or at regularly scheduled clinic visits. Survey questions were read to participants and responses were recorded. Questions regarding reasons for inability to access marijuana, reasons for marijuana use and method of marijuana use were open-ended and all answers were recorded and then categorized. For questions regarding the comparisons of IM to MM subjects were asked to answer either agree, disagree, or don't know. Rates of opioid use, reasons, frequency, and methods of marijuana use before and after obtaining MM were compared using Fisher's exact test.
Results:
Subject Demographics: Our clinic serves approximately 150 patients, 50 of whom have been certified for MM. 27 subjects were offered the survey and 24 chose to participate. Of those who participated 12 (50%) have been able to obtain MM from a dispensary. Those who obtained MM were 29.7 ± 7.8 (mean ± SD) years old and 42% female. Those who did not obtain MM were 37.8 ± 15.3 years old and 50% female. When asked why they were unable to obtain MM 67% noted the cost of certification and 33% noted challenges with the application process. Prior to certification 79% used IM. Of those who had not accessed MM after certification 64% reported using IM, and of those who had accessed MM 44% reported also using IM.
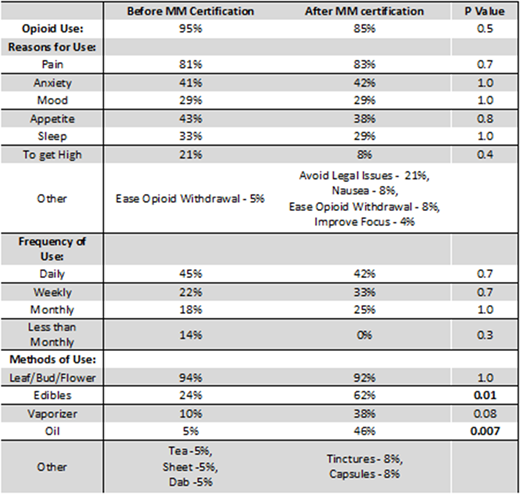
Reasons for, frequency, and methods of marijuana use: The reasons subjects reported using IM were similar to the reasons they reported requesting MM certification (Table 1). Those who obtained MM used at the same rates as subjects had previously used IM (Table 1). Though subjects who obtained MM continued to have high rates of leaf/bud/flower use, they were more likely to also utilize ingestible products such as oil and edibles (Table 1).
Changes in marijuana and opiate use: After obtaining MM 58% felt they had less pain and 53% reported they used less pain medication. However, there was no change in rates of reported opioid use after obtaining MM (Table 1).
Comparisons of IM and MM: When asked questions comparing MM to IM 92% of participants felt that MM was safer, and 92% noted it was less likely to cause legal toxicity. 46% of patients felt MM was stronger than IM and 31% did not. 62% of subjects felt MM controlled their symptoms better than IM. However, 39% of subjects felt that MM was less convenient than IM (31% felt it was not and 31% did not know) and 62% of subjects felt that it was more expensive.
Conclusions: To our knowledge this is the first report of medical marijuana certification in a SCD clinic. One third of our patients requested MM certification, the majority of whom were already utilizing IM. They used MM for similar reasons and at similar rates as they had previously used IM. Once MM was obtained patients were more likely to use oral marijuana such as edibles and oil. Oral marijuana may be preferable to inhaled due to decreased risk of lung toxicity. Patients also reported that MM was better for their pain, allowed them to reduce pain medication use, and was safer than IM. Cost of MM was both a barrier to obtaining access and to purchasing IM. In conclusion, certifying patients for MM appears preferable to patients and may be associated with an improved safety profile.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal